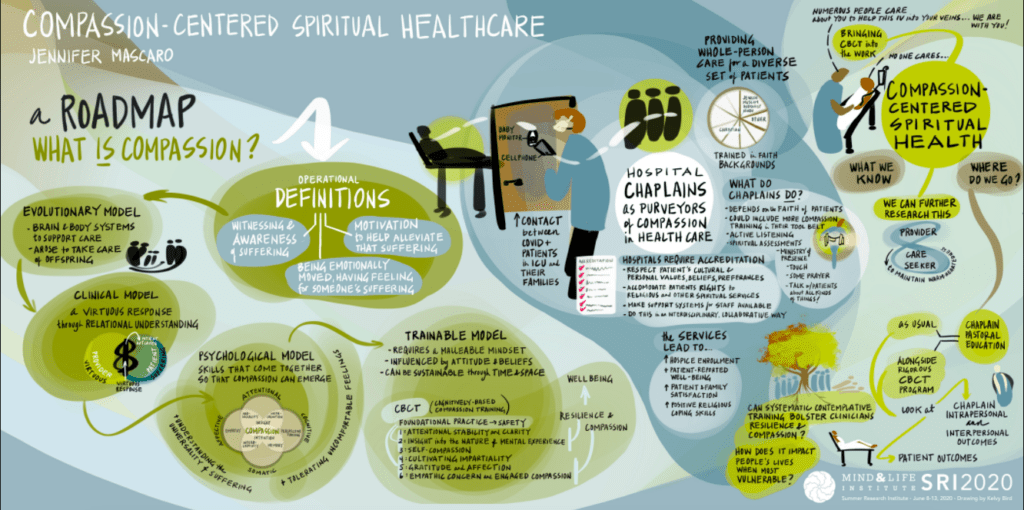
In the midst of the COVID pandemic, health care is in the news daily. But there’s an often-overlooked element in many hospital systems: the role of chaplains. For patients experiencing loneliness, isolation, fear, and physical pain, chaplains offer much needed emotional support, spiritual guidance, and hope.
But could chaplains and the patients they support also benefit from compassion training? In search of an answer, Jennifer Mascaro, a biological anthropologist in the Department of Family and Preventive Medicine at the Emory School of Medicine, and research partner Charles Raison, received a 2017 Mind & Life PEACE Grant. Their study sought to explore whether Emory’s Cognitively-based Compassion Training (CBCT®) could be used—not only to reduce anxiety and strengthen emotional resilience among chaplains—but to enhance the well-being of their patients.
Their research reflects a whole person approach to healthcare that views the physical, emotional, and spiritual needs of patients as integrated, while also seeking to mitigate the stress and burnout experienced by caregivers.
While results from the Mind & Life-funded randomized trial are still being analyzed, in June, Jennifer’s research received a major boost in the form of a five-year K01 career development award from the National Institutes of Health (NIH). The NIH funds will support the evaluation of a chaplain-delivered CBCT® meditation program for patients undergoing cancer treatment.
The award will provide Jennifer and her team with “protected time” to focus on their research without the pressure to fundraise. “The PEACE Grant allowed us to collect pilot data that we used for the NIH grant,” says Jennifer. Her experience is not uncommon. Since 2004, Mind & Life has awarded $5.2 million in grants, with grantees going on to generate more than $110 million in follow-on funding from other sources.
Jennifer’s interest in the benefits of contemplative practice was piqued when she began meditating in high school. The question of how such practices nurture caring for others would inform her academic path and subsequent research. Her current work falls within what is known as implementation science. Over the long-term, the team is looking at how to embed evidence-based contemplative approaches within the workflow of hospitals for the benefit of both providers and patients.
Over the long-term, the team is looking at how to embed evidence-based
contemplative approaches within the workflow of hospitals
for the benefit of both providers and patients.
“There’s lots of discussion around empathy and compassion in healthcare and specifically around burnout,” says Jennifer. “It’s clear that healthcare providers are struggling, which impacts their ability to maintain compassion and empathy for patients.”
With chaplains serving as natural purveyors of compassion in hospitals, it made sense to study how contemplative practice could strengthen their emotional resilience and clinical work with patients. According to one study, contemplative practice comprises less than one percent of the services chaplains provide. Such findings, “pointed to a place where we might be able to bring more tools to a chaplain’s toolbelt,” says Jennifer.
For 15 years, researchers at Emory have been studying the effects of CBCT®, which is derived from the Lojong tradition of Tibetan Buddhism. Among its benefits, the program has demonstrated effectiveness in enhancing compassion among medical students, increasing hope among adolescents in foster care, and reducing rumination and depression among cancer survivors.
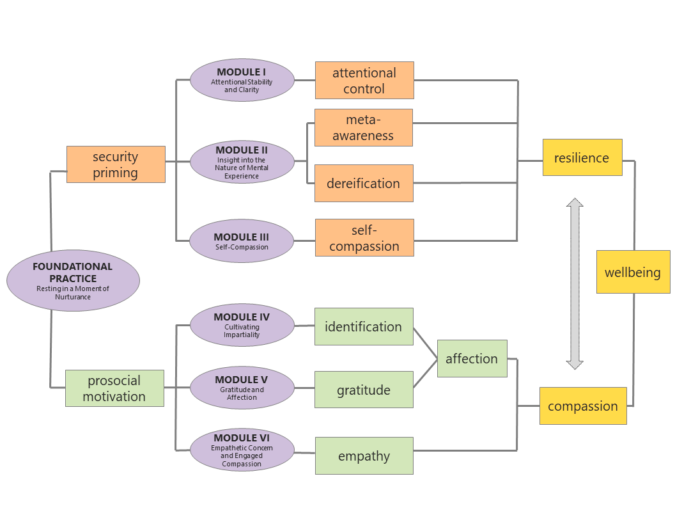
To explore its potential to benefit chaplains, Jennifer and her team incorporated CBCT® into Emory’s clinical pastoral education program. Over four years, 80 chaplains-in-residence have undergone the training. CBCT® begins with a foundational practice to cultivate feelings of safety and appreciation. Participants place their attention on a moment of nurturance, often a memory of when they felt cared for or secure. The program’s six training modules are then delivered over eight to ten weeks. Throughout, the goal is to cultivate impartiality, gratitude, and connection “through which compassion naturally arises,” Jennifer explains.
Preliminary analysis of study data suggests that CBCT® may reduce chaplains anxiety levels and contribute to enhanced well-being. “They feel more emotionally-grounded and less anxious before they see patients,” says Jennifer.
The researchers found that the CBCT®’s benefits also extend to the patients that chaplains support. One chaplain shared the story of a woman who felt abandoned and lonely. Drawing from his CBCT® experience, he suggested that she focus her attention on the various people who make life-saving interventions, such as her IV, possible. The patient’s perspective shifted as she realized the expansive circle of care around her.
As a next step, the Emory team developed a new patient-centered version of CBCT® called Compassion-Centered Spiritual Health (CCSH). CCSH begins with a set of exercises that a chaplain completes before meeting with a patient. The chaplain and patient then work together, through a process of attunement, to access compassion for the patient, along with warm-heartedness and resilience, that can be sustained.
A randomized study found patients who received CCSH reported higher levels of satisfaction, and lower levels of depression and anxiety, than those who received standard pastoral counseling. Yet questions remain. What attributes do chaplains bring that contribute to successful outcomes? What language is most effective?
With funding from NIH, Jennifer will further assess the effectiveness of CCSH. This time, CBCT®-trained chaplains will work with cancer patients receiving hematopoietic stem cell transplants. The researchers will study the effects of CCSH on patients who are hospitalized for two to three weeks, making them particularly vulnerable to feelings of loneliness and disconnection.
Over the long-term, the Emory researchers seek to explore what it takes to apply a new approach—in this case compassion-based contemplative training—within different domains. Jennifer frames it this way: “If you take contemplative science to a new place and deliver it, what does the process look like? How do you study it so that it’s acceptable and feasible?”
It’s a process that takes persistence over time, with the end goal being a more compassionate healthcare system that nurtures the well-being of patients and providers alike.